
What do the latest numbers reveal?
- close to 37 million people are living with HIV
- 95% are adults
- 5% are children under the age of 15
- only about 21.7 million of HIV infected individuals are on antiviral drugs
- if they are not on drugs, they can certainly act as a source of HIV to others
- 940,000 people died from AIDS-related illnesses in 2017!
- About 25% of infected people did not know they had HIV!
How is HIV transmitted?
- Sexually
- basically any kind of sex where mucus membrane or torn skin comes in contact with infected bodily fluids such as semen, blood, vaginal secretions etc.
- from mother to child
- in utero (baby will be born with HIV)
- by breastfeeding, as breastmilk can carry HIV
- during natural childbirth by being exposed to mother’s infected blood
- Accidental exposures
- could be an accidental needle stick injury
- when healthcare providers accidentally stick themselves with a needle containing contaminated blood
- transfusion of contaminated blood and blood products
Who should get tested for HIV?
- The US preventive services task force recommends that all individuals between 13 and 64 years, should get tested.
- People outside this age range should get tested if
- newly diagnosed with a sexually transmitted infection
- they have new sexual partners
- pregnant, including those in labor who are untested and with unknown HIV status

What can you tell a person who is HIV infected?
- it is a managed condition
- infected individuals should stay on a regimen of 3 or more antiretroviral agents
- HIV is no longer the death sentence it used to be at the beginning of this pandemic and that is because we have great drugs that specifically kill the virus.
- But if you don’t get tested, you miss out on treatment.
- Treatment can be expensive, but here in the United States, we have toll-free State HIV/AIDS Hotlines that will connect you with agencies offering programs and services for which you may be eligible.
- compliance is critical to prevent drug resistance
- receive age-appropriate vaccinations that will help prevent vaccine-preventable infections
- practice safe sex practices
- compliance is critical to prevent drug resistance
- HIV is no longer the death sentence it used to be at the beginning of this pandemic and that is because we have great drugs that specifically kill the virus.
What does HIV do once it enters the body?
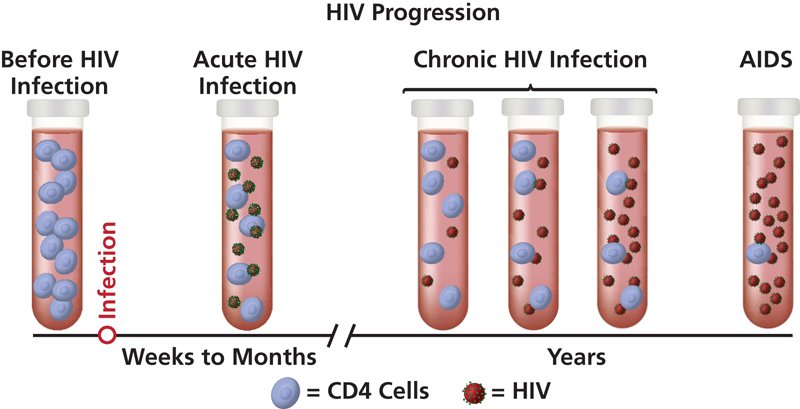

- In 2 to 4 weeks after infection (acute stage), some people show flu-like symptoms (fever, headache, rash).
- HIV seeks and attacks immune cells carrying receptor molecule CD4 and co-receptor molecule CCR5.
- HIV levels in blood are very high – several million viral copies/mL of blood.
- high risk of infecting others
- After the acute stage, is the chronic stage.
- HIV continues to multiply, but at very low levels – may be 50,000 copies/ml.
- There may not be any symptoms at all.
- There is still a risk of passing HIV to others.
- Without treatment, chronic stage will worsen to AIDS in about 10 years or so.
- AIDS is fatal without treatment.
- It takes about 6 months after treatment for HIV levels in blood to become undetectable.
- This helps prevent transmission to others via sex, needle sharing, and from mother to child.
- This is “treatment as prevention”.
- This helps prevent transmission to others via sex, needle sharing, and from mother to child.
HIV and C sections
HIV-positive pregnant women can spread HIV to their babies in utero (in the womb), during delivery and/or by breastfeeding.
The American College of Obstetricians and Gynecologists makes recommendations to reduce the risk of HIV transmission from pregnant women to their babies:
- IF the HIV status of pregnant woman is unknown, she should get tested for HIV at the initial prenatal visit.
- if she is HIV-positive, test her HIV levels (# of HIV copies per mL of blood = her HIV viral load)
- if she is on treatment and HIV levels are undetectable, that is great news
- it means risk of HIV transmission to fetus is extremely low
- she should be monitored every 3 months to ensure undetectable viral load
- it means risk of HIV transmission to fetus is extremely low
- if she is on treatment and HIV levels are undetectable, that is great news
- if the HIV-positive pregnant woman is not on treatment, she should be put on a treatment regimen
- her viral loads should be determined monthly until viral load becomes undetectable
- she should then be tested every 3 months to ensure undetectable viral load
- her viral loads should be determined monthly until viral load becomes undetectable
- if the pregnant woman has a viral load greater than 1,000 copies/mL and she is at or close to delivery, she should be offered a scheduled prelabor C section, to reduce risk of transmission during delivery
- this should be done even if she is on a treatment regimen, but has a viral load greater than 1,000 copies/mL
- she should also be given intravenous HIV meds, before the C-section and until delivery to reduce risk of transmission
- Screening for HIV is done at every pregnancy.
- For more in-depth information, click HERE.
- if she is HIV-positive, test her HIV levels (# of HIV copies per mL of blood = her HIV viral load)
What can we do for infants born to HIV infected mothers?
- HIV-positive infants should receive a drug called zidovudine for 4 to 6 weeks after birth.
- They should be tested for HIV at the following times:
- 14 – 21 days of life
- 1 to 2 months
- 4 to 6 months
- Infants are considered HIV-negative if tests 2 and 3 above are negative.
- Infants are considered HIV-positive if 2 of the above tests are positive.
- HIV-positive infants should now receive combination therapy (instead of zidovudine alone).
- In the United States, women with HIV are counseled not to breastfeed their babies as infant formula is considered to be a safe and healthy alternative to breast milk.
- HIV-positive infants should now receive combination therapy (instead of zidovudine alone).

We do screen our blood supply for HIV. Click HERE to access the United States FDA recommendations for reducing the risk of HIV transmission by blood and blood products. These recommendations were last updated on Feb. 5, 2018.
- The Red Cross screens all donated blood and blood products for HIV-1 (this HIV species is found worldwide) and HIV-2 (confined mostly to West Africa).
- Currently, there is still a small risk of HIV-1 transmission through donated blood.
- This risk is about 1 in a million per transfused unit of blood and/or blood products.
- Currently, there is still a small risk of HIV-1 transmission through donated blood.
How often should we screen for HIV?
- A one-time screening will allow us to identify those who are infected.
- Individuals should undergo repeat screening IF
- at higher risk of HIV infection,
- actively engaged in risky behaviors,
- live or receive medical care in a high-prevalence setting
- high-prevalence setting is a geographic location or community where at least 1% of the community is HIV positive
- These settings include sexually transmitted disease (STD) clinics, correctional facilities, homeless shelters, tuberculosis clinics, clinics serving men who have sex with men, and adolescent health clinics with a high prevalence of STDs.
- high-prevalence setting is a geographic location or community where at least 1% of the community is HIV positive
Why is treatment important?
HIV takes an unpredictable turn once it is inside the human body. It either starts replicating right away, in which case you will start seeing symptoms in a few days to weeks or it stays dormant inside some immune cells. At this time, we cannot predict why HIV will replicate, or stay dormant. We also cannot predict when and why the dormant virus will now start replicating and create issues for the infected person. HIV attacks important cells in our immune system.

- If we allow HIV to make more copies of itself, we allow immune cells to be destroyed by the virus.
- This results in dangerously low levels of immune cells, making the person vulnerable to even the most harmless of infections – the definition of AIDS (acquired immune deficiency syndrome).
- These HIV infected individuals with “detectable virus loads” in their bloodstream are also able to spread the virus to others by –
- sex, needle sharing, in utero, breastfeeding, and blood and blood products.
- IF we put the newly diagnosed person on treatment right away, we are doing two things:
- preventing progression from HIV infection to AIDS, by keeping virus numbers down and
- decreasing or minimizing (not eliminating) transmission
Can we prevent AIDS?
Absolutely, yes.
- We can do this if we are able to diagnose people with HIV and then put them on a therapeutic regimen of antiretroviral drugs.
What is treatment for someone with an HIV infection?
- genetic testing to detect drug resistant HIV (if present)
- 3 or more antiretroviral agents from 2 or more drug classes
- regular testing to
- ensure success of therapy
- success is undetectable viral load
- detect HIV that might develop drug resistance
- ensure success of therapy
- age-appropriate vaccinations

What do HIV drugs target?
- an HIV protein (called GP41) that allows the virus to fuse with certain immune cells – a necessary prelude to entering these cells
- CCR5, a co-receptor that is present on the surface of some immune cells
- if blocked, HIV cannot enter these cells
- reverse transcriptase, an enzyme that is absolutely essential for HIV to make more copies of itself
- when you block this enzyme, you prevent HIV from making more copies of itself
- protease, an HIV enzyme that is essential for HIV to make more copies of itself
- HIV cannot replicate without this enzyme
- integrase, another essential HIV enzyme
- HIV cannot replicate without this enzyme

WHY do we give so many drugs at the same time?
- HIV has the ability to mutate rapidly.
- Monotherapy (one drug at a time) won’t prevent drug resistance.
- It is highly improbable and therefore unlikely, that HIV will mutate to become resistant to 3 or more drugs at the same time.
What if you get accidentally exposed to HIV?
- get treatment immediately: this is called post exposure prophylaxis (PEP)
- it doesn’t matter how small or how extensive the exposure is, all exposures should be treated with 3 antiretroviral drugs, for a period of 4 weeks
- PEP must be started within 72 hours of possible exposure to HIV.
- get tested
- at intervals of 6 weeks, 3 months, 6 months and a year to make sure that you are HIV negative
Who is at higher risk of HIV infection?
On the basis of HIV prevalence data, the following are at very high risk for new HIV infection:
- men who have sex with men
- active injection drug users
- screen once a year for HIV
The following are at high risk of new HIV infection:
- having sexual partners who are HIV infected
- being bisexual
- engaging in sex in exchange for money or drugs
- having a new sexually transmitted infection
- screen for HIV, every 3 to 5 years
You are not at risk of sexually transmitted HIV IF
- you are not sexually active, or
- are sexually active and in an exclusive mutually monogamous relationship with an uninfected partner

Can we prevent those at high risk of getting HIV, from getting infected?
Yes. We can do this with PrEP (pre exposure prophylaxis).
- PrEP is a once daily pill (Truvada) that is FDA approved for use in HIV-negative adults and adolescents who have a sexual partner who is HIV-positive or an injection-drug-using partner who is HIV-positive.
- It is FDA approved for use in combination with safer sex practices.
- Individuals between the ages of 13 and 24 made up 21% of new HIV infections in the United States in 2016, with 81% of these infections in young men who have sex with men.
- PrEP is highly effective when the daily pill is taken like clockwork (same time every day) AND when the person engages in safe sex practices.
- What is considered highly effective?
- Studies show that PrEP reduces the risk of sexual transmission of HIV by more than 90% when used consistently.
- PrEP reduces the risk of HIV transmission among people who inject drugs by more than 70% when used consistently.
- How long do you have to be on PrEP before you are “safe”?
- You reach maximum protection from HIV transmitted by receptive anal sex, after about a week of daily Truvada use.
- The maximum protection for receptive vaginal sex and for injection drug use is about 20 days of daily Truvada use.
- IF you are on PrEP, do you still have to get tested for HIV?
- Yes.
- You get tested before you go on PrEP and then every 3 months while you are on it.

Is PrEP increasing the risk of other sexually transmitted diseases (STDs)?
- Research studies show higher rates of condomless sex AND sexually transmitted infections such as gonorrhea, chlamydia and/or syphilis in PrEP users.
- these infections may not always have symptoms, but infected individuals are contagious and at risk of complications, unless treated!
Do these data help us in the fight against HIV/AIDS?
- Yes. PrEP is introducing to healthcare, those at-risk adolescents and adults who may not otherwise seek care because of perceived stigma or reluctance to be “outed”.
- Research data reveal a greater need for counseling our PrEP users about
- safe sex practices, the very real risk of HIV & other STIs, along with efforts to test and treat
HIV opinion summary
There are over 30 million people living with HIV, globally and about 9 million of these infected individuals are unaware of their HIV status, with 15 million not even on life saving antiretroviral drugs!
- Undiagnosed and untreated individuals add to the HIV contagion.
- Closer to home, over 1.1 million people are living with HIV, in the United States.
- One in seven of these infected individuals are unaware that they are infected.
- Diagnosis of all infected individuals and treatment with antiretroviral therapy is imperative –
- in time, therapy will reduce viral numbers in blood to undetectable levels –
- with continued therapy, these individuals have effectively no risk of transmitting HIV sexually or from mom to infant.
- in time, therapy will reduce viral numbers in blood to undetectable levels –
Of the 39,782 people diagnosed with HIV infection in the U.S. in 2016, about 68% were men who have sex with men (MSM).
- The high risk of HIV infection in MSM may be attributed to unprotected anal sex, having multiple sexual partners, use of alcohol and drugs as a common component of socializing, and homophobic discrimination, which prevents MSM from accessing HIV services.
- We have all seen the billboards, the commercials on TV, and the buses touting HIV services!
- Yet, we are clearly still not able to deliver this crucial message of prevention to thousands of vulnerable individuals.
- We have all seen the billboards, the commercials on TV, and the buses touting HIV services!
December 1, 2018 marked 38 years of this day being commemorated as World AIDS day. AIDS, short for acquired immune deficiency syndrome, is what lays in wait if HIV is untreated. AIDS is a condition marked by high virus numbers in the body and increasing destruction of immune cells. Dangerously low numbers of immune cells make the person vulnerable to any infection, even the usually harmless ones. Once infected, staying on antiretroviral therapy is a life long commitment. In an era where people are living longer, often patients with HIV have to be on additional medications for other chronic conditions, making drug interactions a serious consideration.
- In 2012, the FDA approved Truvada, a daily pill that is over 90% effective at preventing HIV, if taken like clockwork.
- Truvada was approved in combination with safe sex practices, to reduce the risk of sexual transmission in HIV negative, at-risk adults whose sexual partners were HIV positive.
- This is called PrEP, short for pre exposure prophylaxis.
- In May 2018, FDA extended the use of Truvada to at-risk adolescents –
- a smart decision since individuals between the ages of 13 and 24 made up 21% of new HIV infections in the U.S. in 2016,
- with 81% of these infections in young MSM.
- a smart decision since individuals between the ages of 13 and 24 made up 21% of new HIV infections in the U.S. in 2016,
A 30 day supply of Truvada costs close to $2,000, a cost not necessarily conducive to widespread use.
- However, in December 2017, Florida Surgeon General Celeste Philip mandated that all Florida county health departments offer PrEP at no cost by the end of 2018.
- The timing of this mandate was not accidental.
- In 2017, Florida had the highest number of new HIV diagnoses in the country!
- Four of the 10 metropolitan areas with the highest rates of new HIV infection per 100,000 are in Florida:
- Miami (at # 1), Fort Lauderdale (# 2), Orlando (# 6) and Jacksonville (#9).
- Four of the 10 metropolitan areas with the highest rates of new HIV infection per 100,000 are in Florida:
- A word of caution regarding Truvada: it does not prevent other sexually transmitted infections (STIs).
- Research also shows increased rates of condomless sex and other STIs in PrEP users.
- We need to step up our efforts to counsel at-risk adolescents and adults in safe sex practices, the very real risk of HIV and other STIs, along with efforts to test and treat for STIs.
- Research also shows increased rates of condomless sex and other STIs in PrEP users.
In addition to free PrEP in high risk groups, we have to do more, so all at-risk individuals receive appropriate screening, counseling, and other HIV services that will enhance their chances of not being infected.
Preventing HIV is a gargantuan task and I believe it is going to take the entire village to do it right.
CALL TO ACTION
- This December, let’s make a commitment to raise awareness about
- PrEP,
- getting tested and treated,
- safe sex every time (unless you are in a mutually monogamous relationship and both partners are HIV negative),
- not bowing to peer pressure and engaging in unsafe sex,
- preventing sex trafficking,
- preventing injection drug use,
- supporting safe syringe programs, and
- educating everyone about prevention.
- Let’s talk prevention with those closest to us –
- our friends, co-workers, siblings, children, grand children or maybe even our parents and grandparents.
- Let’s partner with community organizations by donating, time, money and/or our expertise.
- Together, and with a concerted effort, we truly can stop HIV.